From racing shoes to headlamps and everything in between, runners can be quite picky about their gear. As time goes on and technology advances, runners want the best of the best to be able to perform well, stay away from injury, and recover as fast as possible. Believe it or not, socks play a significant role in foot health for athletes. They are not just made to add a layer of cushion in between the skin and shoe seams. They can provide the feet, and pretty much every joint up the body, with support and injury prevention no matter what your lifestyle dictates.
Comfort is Always Number One
The first thing we aim for when picking out any piece of an outfit, shoes, or socks, is comfort. Runners, in particular, don’t care as much about looks, as long as they can feel comfortable on their long runs and avoid issues like achy joints, blisters, and heaviness. This all can be solved with a good pair of socks. In comes Apolla Performance. Initially created for dancers, who we can all agree get the most beating to their feet, these styles are equally perfect for any lifestyle. Just recently a research study concluded their effectiveness in reducing force and received the American Podiatric Medical Association Seal of Acceptance.
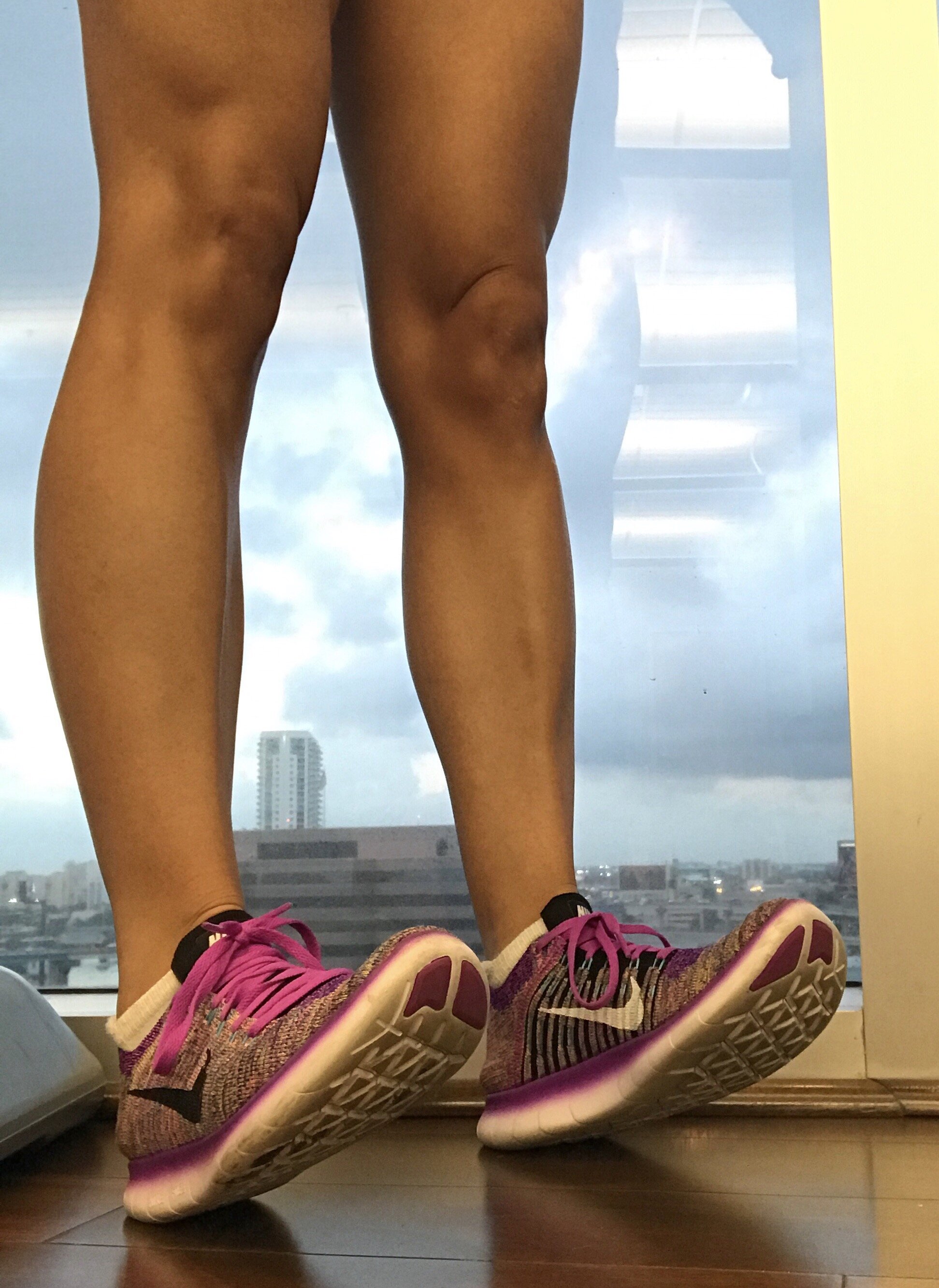
Apolla Performance socks are all made in the USA with REPREVE, which is certified sustainable yarn. Runners are sure to be happy with the Amp (no-show), the Performance (crew), and the Infinite (mid-calf), since they all provide the perfect thickness to protect from impact, blisters, and moisture, without feeling suffocated in running shoes. Each has energy absorption padding in the heel and ball of the foot which helps cushion during both push-off and landing—the parts of the running cycle that damage the feet the most. If you suffer from plantar fasciitis, you will be grateful for this feature!
Instability is the Enemy
As a physical therapist, I am an advocate for creating the most stable surface during the running cycle. This means being extra picky about the shoes and socks you wear. Weak, overused, or tired ankle and foot muscles can lead to ankle rolls and strains in the tiny muscles of the foot from the constant work when your foot and ankle are not supported well. Apolla Performance socks are made with targeted high compression where you need it the most—around the ankle joint and the arch of the foot. The arch actually has three zones of compression to lift and stabilize, which makes a significant difference if you suffer from plantar fascia issues. In these cases you want to prevent your arch from getting too stretched out, which will end up tugging on your heel bone. It’s a tough condition to treat, so you want to do anything you can to avoid too much pressure to this area!
Work Hard, Recover Harder
The mid-calf Infinite Sock from Apolla Performance is the best choice for both recovery runs and your rest days. Providing your feet and lower legs with compressive support is ideal to help with circulation—the key to recovering faster. This is best done with graduated compression up the calf, which is exactly what this pair provides. Using compression socks during and after runs, especially speed workouts and long runs, is ideal for those suffering from achy calves, shin splints, Achilles tendinitis, and any other foot and ankle conditions. You want good blood flow and comfortable cushioning if you want to be fully ready for your next workout. If you are looking for happy and healthy feet, Apolla Performance has you covered!